Kristin Claricoates, DVM
A cardiomyopathy is a descriptive condition where the muscles of the heart is abnormal. There are four types of cardiomyopathies: “hypertrophic”, “dilated”, “restrictive” and “right ventricular”. While hypertrophic cardiomyopathy, or HCM, has typically been recognized by its structure i.e., thickening of the heart muscle, the electrical function of the heart is also adversely affected.
The main feature of hypertrophic cardiomyopathy is an excessive thickening of the heart muscle (hypertrophy literally means to thicken). The distribution of muscle thickening or hypertrophy is variable, but the left ventricle is almost always affected and in some patients the muscle of the right ventricle also thickens. In HCM, the walls of the heart or the septum separating left from right chambers of the heart are thickened. HCM can sometimes be confused with a heart that appears similarly, but is a normal change in the heart in individuals with high blood pressure (hypertension).
In Hypertrophic Cardiomyopathy (HCM), the muscle thickening occurs without an obvious cause. Examination of the heart muscle in Hypertrophic Cardiomyopathy under a microscope shows that the normal parallel alignment of muscle cells has been lost. The cells appear disorganized. This abnormality is called “myocardial disarray”. It is probable that myocardial disarray interferes with normal electrical transmission and predisposes to irregularities of the heartbeat.
Myocardial Disarray
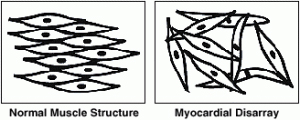 These diagrams contrast the regular, parallel alignment of muscle cells in a normal heart with the irregular, disorganized alignment of muscle cells or “myocardial disarray” found in some parts of the heart in hypertrophic cardiomyopathy.
These diagrams contrast the regular, parallel alignment of muscle cells in a normal heart with the irregular, disorganized alignment of muscle cells or “myocardial disarray” found in some parts of the heart in hypertrophic cardiomyopathy.
When a heart is in HCM, the thickened muscle usually contracts (pumps blood) well and ejects a higher than normal amount of the blood from the heart. However, the muscle in HCM is stiff, so it is unable to relax completely. As a result, higher blood pressures compared to normal are required to fill the heart. The amount of blood which the heart can hold is therefore reduced. This in turn will limit the amount of blood which can be ejected with the next contraction. While the heart itself has problems with thickening of the musculature, the heart valves and arteries are normal. Normally, the heart is set up to process unoxygenated blood and make it oxygenated to send to the tissues of the body. There are four chambers of the heart and four one way valves to continue pumping blood in this uni-directional process. The right atrium receives blood from the body which is poorly oxygenated, sends it to the right ventricle, where it is then transferred to the lungs. Blood becomes oxygenated and carbon dioxide is expelled. From there, the blood goes to the left atrium, then to the left ventricle, which pumps it to the body. This cycle is continuously repeated as the heart beats. Every heartbeat results from an electrical signal starting at the right atrium and travels down through the heart through special conducting tissue which starts a contraction. In a heart with HCM, not only are the muscles of the heart thickened, but this change can sometimes interfere with this normal electrical signal. Some of the different types of electrical signal malfunctions are arrhythmias of differing severities. These electrical malfunctions can even cause a cardiac arrest.
In an HCM heart sometimes the “plumbing” in the heart can cause the fluid (in this case blood) to get blocked temporarily while attempting to leave the heart (obstruction). This type of a “plumbing” problem should not be confused with blocked arteries in the heart – that is coronary artery disease and NOT HCM.
Hypertrophic Cardiomyopathy may be suspected because of symptoms, a murmur, or an abnormal radiograph. Because such symptoms could be caused by a large number of other conditions, an ultrasound is required to officially diagnose hypertrophic cardiomyopathy. If an arrhythmia is heard, an ECG may be recommended as well. An ECG records the electrical signals from the heart and is performed by placing electrodes in the armpits and inner legs. In Hypertrophic Cardiomyopathy the ECG usually shows an abnormal electrical signal due to muscle thickening and disorganization of the muscle structure. Some patients may only show minor changes or be normal on an ECG. Because ECG abnormalities are not specific to Hypertrophic Cardiomyopathy and may be found in other heart conditions, an ECG may or may not be done depending on the stress level of your pet.
To officially diagnose HCM, an ultrasound of the heart is needed. This is sometimes an echocardiogram, or an ECHO. An ECHO produces a picture of the heart, and if excessive thickness of the muscle can be seen, HCM is diagnosed. During the test the entire heart is measured including the walls, valves and other structures within the heart. Therefore ECHO provides a very thorough assessment of Hypertrophic Cardiomyopathy, and it can differentiate HCM from other heart conditions that may be suspected.
Because HCM develops over a period of time, your pet may not be exhibiting any signs of HCM because the change in the heart began slowly. Things that may indicate HCM in your pet, or a worsening of HCM can be breathing decreased appetite, weight loss, and an increase in respiratory rate. Loss of energy and appetite and reduced exercise may be seen, but can go unnoticed because pets are often able to recognize their own physical limitations and restrict their activities accordingly.
Drug treatment or medication is given when some or all of the symptoms listed above are present. These medications must be given for the remainder of your pet’s life, and the heart will be evaluated by alternating bloodwork and radiographs every 3 months. Increasing, decreasing or discontinuing medication should only be done with consultation with your veterinarian. The choice of treatment will vary from individual to individual but the common drug groups used for treatment medications are listed below:
Beta-Blockers
Beta-Blocking drugs slow the heart beat and reduce its force of contraction. Beta blockers have such names as atenolol, and sotalol and the names normally end in “ol”. Beta-blockers are also widely used in medical practice for other types of heart disease and for high blood pressure. Occasionally excessive heart rate slowing with these drugs can cause reduced energy
Calcium Antagonists
The second major group of drugs used are the calcium antagonists or calcium channel blockers. Within this group diltiazem is the drug which has been most commonly used in HCM in our patients. It improves the filling of the heart. Like beta-blockers it can cause excessive slowing of the heart rate and lower blood pressure, which is why regular checkups are required to check the heart.
Anti-Arrhythmic Drugs
These drugs might be used when an arrhythmia (irregular heart beat) such as tachycardia (heart beating too fast) is detected and felt to be important in an individual case. Sotolol is a very helpful medication for those who encounter arrhythmias. It may lower blood pressure and appears to have few side effects.
Other Drugs
There are a number of specific complications described earlier which are rare but which require the use of additional drugs.
Diuretics
Occasionally patients develop fluid retention and in these situation diuretics “water pills” which increase urine flow are administered. The most commonly prescribed diuretic is Furosemide (Lasix). It is also imperative to maintain an appropriate blood potassium level when taking diuretics.
Anticoagulants: These are not used commonly in our patients but can be used in patients with atrial fibrillation to prevent clot formation in the atria. Warfarin (Coumadin) is the tablet commonly used with a long history of success in HCM. It requires monitoring with a blood test, approximately on a monthly basis.
Antibiotics
Although endocarditis is rare, persons who have out flow obstruction and turbulent blood flow should receive antibiotic prophylaxis prior to dental procedures (including cleanings) and any other situations where there is an increased risk of bacteria entering the bloodstream.
There are a variety of drug treatments currently used in Hypertrophic Cardiomyopathy (HCM). The need for any treatment and choice of that treatment has to be made on an individual basis and may change in each patient over the years. It is very important to discuss your pet’s symptoms with the veterinarian and develop a treatment plan for your pet, as each patient with Hypertrophic Cardiomyopathy (HCM) is different. Medication should NEVER be stopped without first consulting with your veterinarian. While medications can be stopped some drugs can have a serious complication if stopped abruptly, please work with your veterinarian to manage all medications. You will be doing follow up examinations every 3 months.
Works Cited: The Hypertrophic Cardiomyopathy Association

